The Covid-19 health emergency and the gender gap that exists nationally in the field of palliative and pain medicine led physicians from all over the country to organize to create a space for support among female doctors seeking to improve care for families.
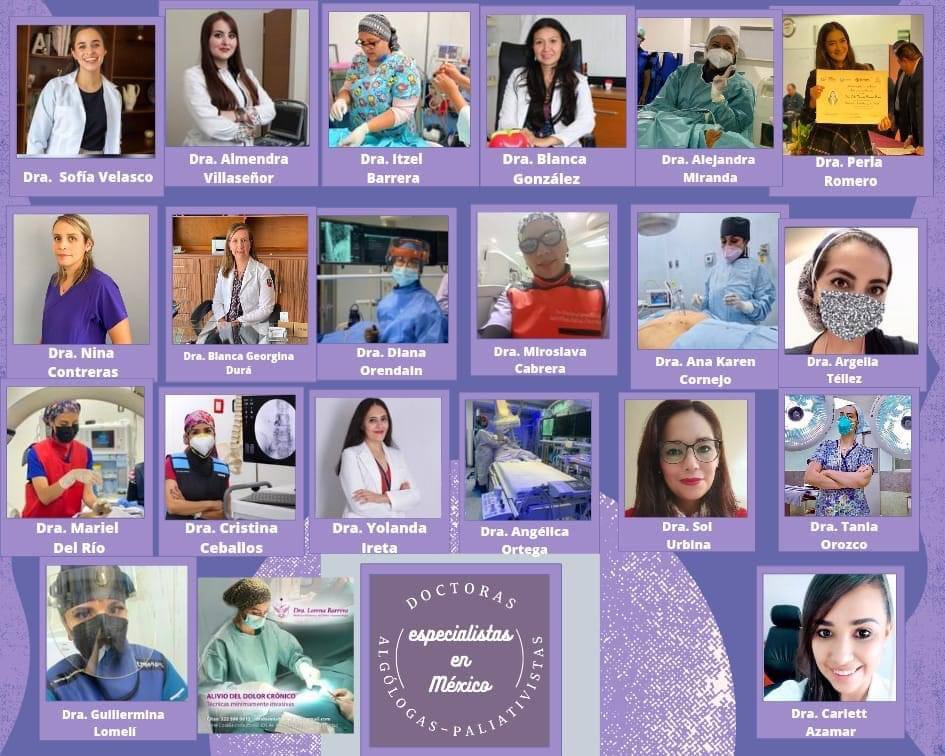
This is an initiative that began to take shape on March 1, and so far includes 36 women specialists in Guadalajara, Zacatecas, Sonora, San Luis Potosi, Michoacan, Colima, Guanajuato, Yucatan, Mexico City, State of Mexico, Quintana Roo, Chiapas, Sinaloa, Baja California, Nuevo Leon.
In an interview with Zonadocs.mxDr. Sol Urbina Gutiérrez, an anesthesiologist and specialist in palliative and pain medicine, points out that one of the causes that led them to organize and work together was the COVID-19 health emergency, since the crisis contributed to making visible the overload of care work, especially for women, as well as the limitations that arose in patient care.
He points out that, within the healthcare field, the specialty of palliative and pain medicine is responsible for providing relief from the symptoms and stress caused by serious illnesses.
This specialty focuses on the care of patients with physical limitations who may have an immediate life-threatening condition or whose illness may be prolonged for a long time; it is also responsible for the care of recovering patients.

Urbina indicates that, throughout her career, she has identified that this determines, on the one hand, the visibility and scope that this specialty has and, on the other hand, the scope and positive impact that this could have on the lives of many female patients with a serious disease.
The main barrier identified by the group, he points out, is that there are not enough specialists in palliative medicine in public health facilities. Added to this is the fact that the specialty as such is not known and, therefore, places within the public health system are not prioritized.
Recently, within the private health system, job openings for doctors with this specialty have begun to be offered; this has been the result of the sum of their demands, but there is still work to be done in the public sector.
"The public health system does not give you the security of having a fixed salary or stability, so we look for private spaces," she says.
In addition, she adds, palliative care physicians face gender gaps.
"Sometimes they prefer to hire doctors, because for us they always consider things like whether we already have children, whether we want to have more, or whether we plan to get married, questions they obviously don't ask men."
The initiative arises from a research that investigates the gender perspective within medicine. The text warned that patients attended by female doctors have a more favorable prognosis compared to those who are accompanied by male doctors. The case in question referred to cardiology; however, the doctor explains, it could be applicable to any other specialty, including her own.
From this questioning came others, she acknowledges, such as the cultural impact of machismo and misogyny in the medical practice of palliative care and pain medicine and, therefore, in the health of patients. With these approaches in mind, she contacted other female doctors to get organized, link up and begin to generate spaces as specialists in this area of medicine from a gender perspective.
Now, the idea of forming an organization of palliative medical women has the initial objective of creating a space for growth and support that contributes to generate conditions in the professional, personal and work environment of its members.